“Polio was never the raging epidemic portrayed in the media, not even at its height in the 1940s and 1950s,” David M. Oshinsky writes in Polio: An American Story. Yet at the turn of the 20th century, the public fear of polio reached a fever pitch.
The virus struck seemingly without warning, leaving children, mostly young boys, with varying degrees of paralysis and in some circumstances, death.
The first recordings of poliomyelitis, shortened to “polio” by American journalists who balked at using the 13-letter word, was in Egypt in 1500 BC. However, when polio did strike, for almost everyone the result was usually a mild infection followed by a lifetime of immunity, according to Oshinsky. In later years, little attention was given to it in the press.
Indeed, the first recorded polio epidemic in the United States, which occurred in Otter Valley, Vermont in 1894, would have gone largely unnoticed without the tireless efforts of Charles Caverly, a young country doctor. Tracking down the 123 struck by the virus, Caverly found that 84 cases were under the age of 6, 50 were permanently paralyzed from polio, and 18 died. Most notably, Caverly found that a majority of the victims were male.
By the 1930s, polio had received significant attention from both the press and the medical community. In 1938, with the backing of President Franklin D. Roosevelt, who was diagnosed with polio in 1921 at the age of 39, the National Foundation for Infantile Paralysis was founded. Within that foundation — later renamed the March of Dimes — a fierce competition to develop a vaccine emerged between three people: Albert Sabin, Jonas Salk, and Hilary Koprowski.
Sabin and Koprowski backed the live-virus vaccine, which is designed to create a natural, weak infection that would trigger the body to generate antibodies. But unlike his peers, Salk favored a dead-virus version “intended to stimulate the immune system to produce the desired antibodies without creating a natural infection,” writes Oshinsky. While most polio researchers backed Sabin and Koprowski’s approach, the foundation privately deemed that Salk’s method might be quicker and more marketable. Salk had the edge.
In 1951, Salk and his team had successfully developed a method that cultivated the poliovirus in the kidney tissue of monkeys, giving Salk the ability to produce large quantities of the virus. The following year, he rapidly began conducting the first human trials on children at two Pittsburgh institutions for the physically and intellectually disabled. Salk even went as far as injecting his own wife and three sons with his vaccine. Time was of the essence, as that year alone saw 58,000 new cases of polio, with more than 3,000 Americans dying from the disease.

By March 1953, Salk was ready to announce that he had successfully created a polio vaccine. Salk insisted that “progress has been more rapid than we had any right to expect” but cautioned the public that “no vaccine [was] available for widespread use for the next polio season,” Despite this, the radio announcement was met with widespread jubilation, and the scientist became an instant hero to the American public.
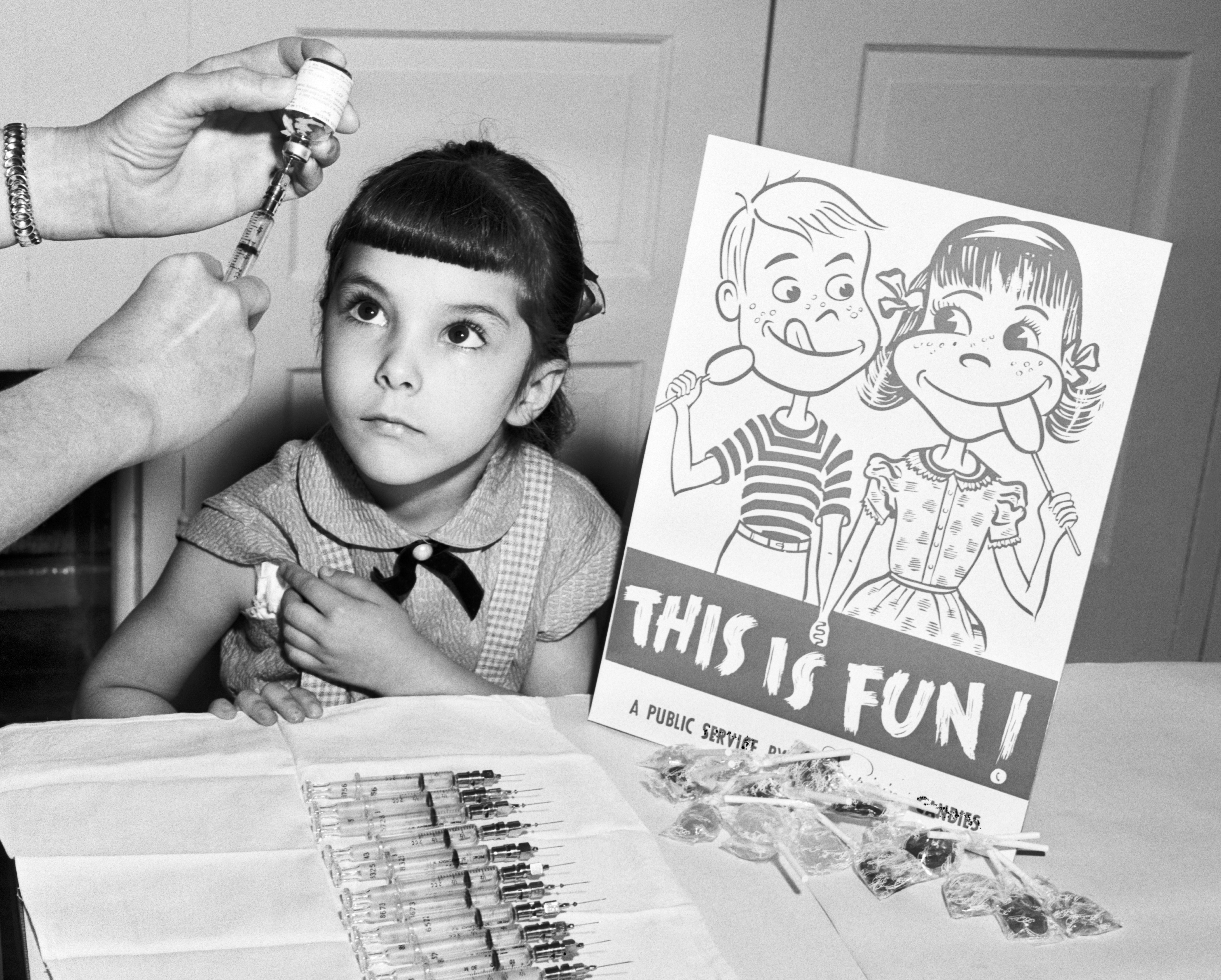
The Vaccine Advisory Committee approved a field test of Salk’s polio vaccine, which commenced the largest medical experiment in American history. The so-called Salk Vaccine Field Trials of 1954 involved almost two million elementary school children, writes Oshinsky. Elvis Presley even volunteered to be vaccinated on live television to encourage others to take the vaccine.
After a year, at a news conference at the University of Michigan, the results of the trial were announced. They vaccine, they said, was 80 to 90 percent effective against the polio virus. That same day, the U.S. government licensed Salk’s vaccine for widespread distribution.
The vaccine did not come without cost, however. Just weeks after the landmark conference, 11 children who were recently vaccinated died and hundreds of others were left paralyzed.
The defective vaccine was traced back to Cutter Laboratories in California, and although unproven, it “is likely that certain production methods (which, it turns out, did not follow Salk’s instructions) resulted in a failure to completely kill the Type 1 (Mahoney) poliovirus in the vaccine,” according to the Historyofvaccines.org.
Others within the scientific community argued that Salk’s vaccine was unsafe and ineffective. Among the loudest of the voices was Sabin, Salk’s fiercest rival.
GET HISTORY’S GREATEST TALES—RIGHT IN YOUR INBOX
Subscribe to our HistoryNet Now! newsletter for the best of the past, delivered every Monday and Thursday.
Yet despite the Cutter incident and initial delays in production, by 1957 new polio cases had dropped to under 6,000 in the U.S. And, according to the Centers for Disease Control and Prevention, no cases of polio have originated in the U.S. since 1979.
For his work, Salk was awarded the two highest civilian honors: the Congressional Gold Medal in 1955 and the Presidential Medal of Freedom in 1977. Salk, however, was notably denied admission to the National Academy of Sciences, with his longtime rival Sabin sneering, “You could go into the kitchen and do what he did.”
Salk is credited with saving the lives of millions and providing all Americans with relatively cheap and widespread access to his vaccine. The scientist never patented his polio vaccine and lost out on billions of dollars in revenue.
In later years, when asked by journalist Edward R. Murrow why he never sought a patent, Salk responded, “Well, the people, I would say. There is no patent. Could you patent the sun?”