Debunking the legend that chemotherapy came from a WWII tragedy
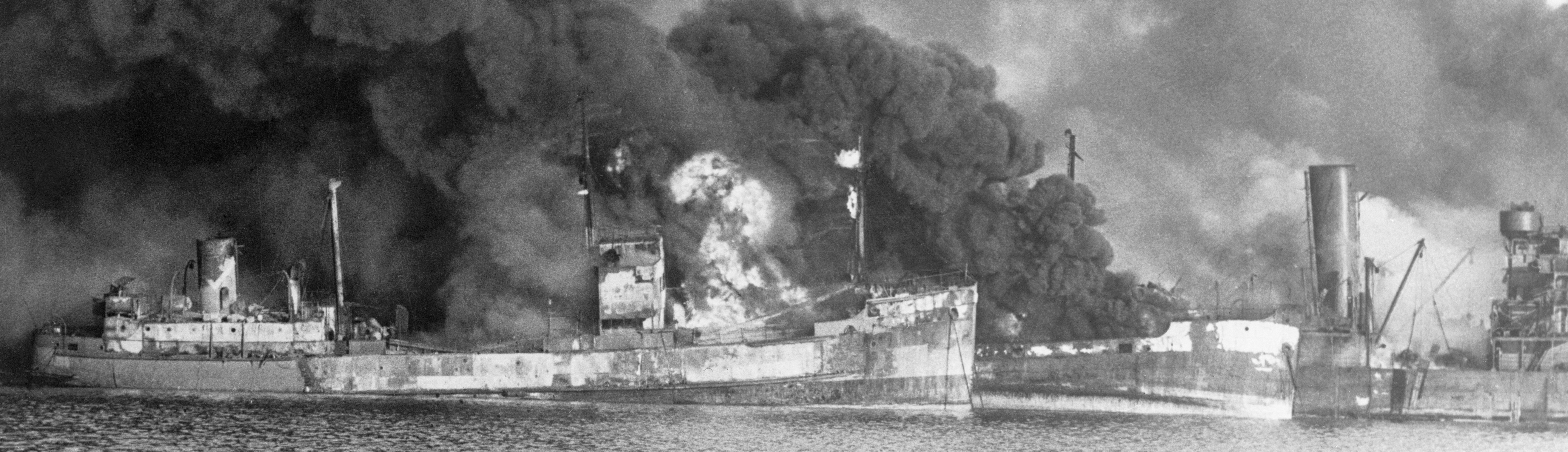
GERMAN PILOTS flying Junkers Ju 88 medium bombers over the Adriatic Sea to attack Bari, Italy, the evening of December 2, 1943, achieved complete and devastating surprise.
Bari was a rich and easy target. Once the British 1st Airborne Division captured the Italian port in September 1943, Bari’s waterfront became a hub for receiving and transferring materiél Allied forces badly needed to take the German stronghold at Monte Cassino, as well as to stage a coming push north to Rome. On the docks stevedores were working day and night, with ships queueing in lines for room to unload. According to Allied intelligence, the Luftwaffe in Italy was under too much pressure to hit Bari hard. So completely did the Allies believe they controlled the vicinity that no fighter squadrons were stationed near the port, which had only rudimentary anti-aircraft defenses.
The afternoon of December 2, a German pilot reconnoitered Bari and realized how ill-protected the harbor was. That aviator’s report prompted General Field Marshal Albert Kesselring, German commander in the Mediterranean war zone, to round up 105 bombers around Italy and Yugoslavia for an immediate attack. That night’s raid surprised 30 Allied transports—American, British, Dutch, Norwegian, and Polish—carrying more than 30,000 tons of supplies. The Ju 88s sank 27 ships along with a civilian Italian schooner, Inaffondabile (“Unsinkable”). Two of the ravaged transports held ammunition; explosions from those cargos shattered windows seven miles away. An oil pipeline on the pier burst, igniting a massive blaze. The attack killed 2,000 military personnel and civilians.
Most perilously, among the vessels destroyed was SS John Harvey, an American Liberty ship. The Harvey was carrying a secret cargo: 2,000 bombs, each packed with upwards of 60 lb. of deadly mustard gas. The ship exploded, releasing a poisonous cloud whose effects eventually hospitalized more than 600 military personnel and struck down uncounted civilians. Within the month, 83 military casualties of the gas had died—some because medical crews, intent on preventing hypothermia in patients retrieved from the frigid harbor, had wrapped patients in blankets, not realizing this act of kindness was pressing oily mustard gas residue closer to their skin.
However, the John Harvey disaster came to be seen as less than a total loss.
During World War I, German use of poison gas proved so effective, injuring 1.23 million, of whom 90,000 died particularly horrible deaths, that in 1925 the nations of the world signed a ban on using gas as a weapon of war.

Even so, Japan maintained a huge chemical warfare laboratory and in China during the 1930s often deployed chemical and biological weapons. The Allies had no certainty that Germany would not do the same in Europe. To be ready to retaliate against such an instance, the U.S. War Department began producing the mustard gas packed into those bombs aboard the Harvey; the 1925 treaty only applied to deploying poison gas, not manufacturing the stuff.
The U.S. Army also began to work to develop an antidote to mustard gas. That effort was well under way at the time of the Bari attack. Hoping to obtain insights from events at the stricken port, the Army dispatched Lieutenant Colonel Stewart Alexander to Italy. Alexander, a physician and chemical warfare expert, was to collect date on mustard gas patients. Autopsies of the dead at Bari showed that the gas had stopped certain cells from dividing. This suggested to Alexander a bodily mechanism that might be harnessed to stop cancer cells from dividing and multiplying.
This optimistic aspect of a disaster secured the Bari raid a place not only in military history but medical history. Again and again the literature outlines how discoveries that Alexander made during autopsies at Bari led directly to the first successful use of chemotherapy to treat cancer in a human being. That single pioneering case evolved into a market expected to reach $148 billion in 2018. National Cancer Institute data show that more than 70 percent of patients in the United States with breast or lung cancer receive chemo. The link between modern chemotherapy and the Bari discoveries appears in such textbooks as 1993’s Cancer: Principles and Practices of Oncology and 1995: Chemotherapy in Clinical Oncology. A 2003 World Health Organization monograph on cancer management states, “The use of chemotherapy to treat cancer began in 1943 following the observation of leukopenia [reduction in number of leukocytes] in military personnel exposed to mustard gas after an explosion of a battleship in Bari harbor.” As recently as 2015, a history of chemotherapy published by biotech research firm Novogen was declaring that Alexander’s autopsy results collected at Bari led to the first chemotherapy trial.
But none of it is true.
Yes, the first successful human chemotherapy trial did use a form of mustard gas. Yes, scientists working for the U.S. Army made that drug. But those events took place 15 months before that pack of Ju 88 pilots raided Bari.
One reason the Bari myth persists is that the story is an epic wartime tale: Nazi bombardiers, gigantic explosions, gruesome mass fatality—and lifesaving therapy arising from, even giving some meaning to, the demise of thousands slain in a horrifying flash. Too good to check, as the saying goes.
However, the Bari myth took hold and held on for a more prosaic reason: wartime secrecy. American researchers used mustard gas-related chemo with success in 1942. However, military authorities suppressed that news until 1946, and even then held back details that left the public case report sketchy, for instance not naming the active ingredient but referring to the formulation as “substance X.” The United States was not alone in its subterfuge; in 1942, the British tried using mustard gas in this way, too, and they hid the resulting data until 1947.
The world learned of that first chemotherapeutic success when the April 5, 1946, issue of Science magazine reported on the case of a 48-year-old bachelor. The man, who lived alone in a rented four-room house in Meriden, Connecticut, had since 1924 worked the day shift at a ball-bearing factory. A native of Poland, he immigrated to the United States at 18. “J.D.,” as the magazine report referred to him, visited New Haven Hospital complaining of an enlarged tonsil. In April 1941 doctors diagnosed a much more serious condition: non-Hodgkin’s lymphoma. A tumor in the lymph nodes lining J.D.’s neck had grown so large—the size of a softball—that he barely was able to open his mouth. Doctors administered the standard cancer treatment: a daily dose of radiation for 15 days. The treatment significantly shrank the tumor. A biopsy showed the cancer cells to be dying.
The effects of radiation lasted eight months. However, despite radiation and surgery, tumors spread to J.D.’s right armpit, becoming so obstructive that to look right or left he had to turn his entire body. He was having trouble breathing. “The patient’s outlook is utterly hopeless,” read an August 25, 1942, note in J.D.’s chart.
Asked to volunteer to be the first to try a new cancer treatment, J.D. jumped at the chance. That possibility had emerged from efforts by the U.S. War Department’s Office of Scientific Research and Development to develop an antidote to poison gas. The office

had had Yale University’s medical school investigate alternatives. Chemist Milton Winternitz, who headed the program, began by working with another poison gas, phosgene. To conduct the mustard gas study, Winternitz recruited colleagues Alfred Gilman, a pharmacologist, and Louis Goodman, a physician and pharmacologist. Gilman and Goodman found mustard gas too volatile to work with, but by adding nitrogen were able to create a compound chemically similar yet stable enough for experiments. Delivered as vapor on a battlefield, mustard gas has a delayed but scarifying effect, causing potentially fatal bleeding and blisters in the lungs and on the skin. On a longer-term basis, mustard gas kills by stopping bone marrow cells from growing. Gilman, Goodman, and associates wondered if they could apply that effect to stop cancer cells from growing. A colleague at Yale’s Department of Anatomy had developed a way to transplant a lymphoma tumor into a mouse. Once in place, the transplanted tumor grew enormous. That scientist gave one of his tumor-laden mice to the poison gas researchers. “We could not wait to get a whole group of animals, so we gave the mustard gas to this one lone mouse, which had a fairly advanced tumor,” Gilman said in 1959. “After just two administrations of the compound the tumor began to soften and regress…The animal lived 84 days following the implantation of the tumor, which was a very remarkable prolongation of survival time.” The mustard gas treatment had worked just as the researchers had hypothesized.
Now the team had to test the approach in humans. Gilman and Goodman recruited Yale assistant professor of surgery Gustaf Lindskog to work with them. “Any drug that gave any promise of controlling malignancy appeared to me to be worth trying, Lindskog told a reporter in 1983. Reviewing his case, team members saw in J.D. a good prospect and made the offer the ball-bearing maker so readily accepted.
Daily injections of the mustard gas-nitrogen compound reversed all of J.D.’s symptoms. By day four of six days of injections he felt better and was eating and sleeping normally. A month after the start of the chemotherapy protocol all signs of tumor were gone. However, the almost magical effect lasted only weeks. A second course of treatments reprised the benefits—for a while. However, a third round had no effect. J.D. died 96 days after starting treatment—96 days he probably otherwise would not have had.
The Science article excited some researchers. “We are on our way to curing cancer,” rejoiced Cornelius Rhodes, president of the Memorial Hospital for Cancer and Allied Diseases in Manhattan. Europeans had made the main breakthroughs in therapeutic use of radiation, for decades the go-to cancer treatment. Now, in terms of chemotherapy, Americans held the lead.
But in the larger medical community chemotherapy “was not widely embraced,” says Vincent T. DeVita, Jr., professor of medicine at Yale Cancer Center. “In fact, the critics were vitriolic about it. People just did not believe you could cure cancer with a drug.”
This resistance partly reflected ingrained ideas of what constituted effective therapy. Doubt also revolved around use of the word “cure.” Paul Ehrlich, the 1908 Nobel Prize winner most famous for discovering the first effective treatment for syphilis, had coined
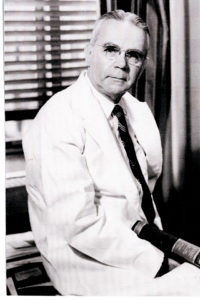
the very term “chemotherapy.” The amazing successes that antibiotics were racking up in the 1940s gave those few who did see promise in treating cancer with drugs hope for a “magic bullet” similar to Ehrlich’s. However, somewhat prolonging a sick person’s life did not project that lustrous aura. Because mustard nitrogen was effective for only a fairly short period, “an air of pessimism pervaded the subsequent literature of the 1950s,” DeVita says, noting that certain prominent researchers “became harsh critics of a national drug development program and the effort to prove that drugs could cure advanced cancers.”
However, investigators working outside the medical mainstream had long been intrigued by the way in which mustard gas halted cell proliferation. Edward Krumghaar, a physician who during World War I treated soldiers in France who had been exposed to mustard gas, reported in a 1919 Journal of the American Medical Association article that among results he found was a profound decrease in circulating white blood cells in patients’ bone marrow. The world noted neither Krumghaar’s finding nor the implication that it might be possible to harness a substance that halted normal cell division to kill cancer cells.
In England during the 1920s, pathologist Isaac Berenblum at the University of Leeds worked with mice in which he had induced tumors. Hoping to irritate the tumors into growing more quickly, Berenblum applied mustard gas. In 1929, he reported that the treatment had the exact opposite effect, inhibiting tumor growth in an “anti-carcinogenic” manner. Building on Berenbluhm’s findings, researchers at New York’s Memorial Hospital reported in 1931 that they had had success treating 13 skin cancer patients with a topical solution of diluted mustard gas. The Memorial Hospital work went no further.
The post-WWII combination of the Bari autopsy data and New Haven Hospital’s results in treating J.D. encouraged a few investigators to look into chemotherapy. Five months after the paper on J.D.’s case appeared, JAMA reported on preliminary results from mustard gas therapy used to treat a total of 67 patients, including seven that the Gilman team treated. These patients had varied cancers, including lymphosarcoma like J.D.’s, Hodgkin’s disease, leukemia, and what the article called “allied and miscellaneous disorders.” Chemotherapy got another major boost in 1948 when pediatric pathologist Sidney Farber at Harvard Medical School reported success using aminopterin, a derivative of folic acid, to treat acute leukemia in children.
In 1955 the U.S. government undertook a coordinated effort to harness drugs in the fight against cancer. Congress established the Cancer Chemo Therapy National Service Center, dedicating $5 million to screening a variety of substances for tumor-fighting properties. The new entity “acted like a pharmaceutical company, using remedies on standardized mice and organizing multi-center clinical trials in hospital units where treatments were free,” explains John V. Pickstone, founder of Britain’s Centre for the History of Science at the University of Manchester. The American center screened more than 11,000 compounds in its first five years. However, according to historians at the National Cancer Institute, the practical contribution to medical practice from this effort was hampered for lack of a road map in the form of “agreement on what models to use, how to use them, or what changes in the tumor constituted activity.”
Even so, by the 1970s the health care system had embraced chemotherapy as a common treatment for cancer—thanks to two realizations, according to DeVita. One was a willingness to try unproven drugs in patients who had had tumors removed surgically but faced a strong likelihood of recurrence. The other was improved understanding of cancer, which scientists now realized was much more complex and varied than syphilis—no single “magic bullet” would stop all cancers, or even cancers of a particular sort. “Take a cancer like cancer of the pancreas,” DeVita said. “There are about 12 different key abnormalities, and you are going to have to make different kinds of combination chemotherapy.” As chemotherapy proliferated, doctors wanted to learn more about the original chemotherapeutic regimen at New Haven Hospital that had helped J.D. However, his patient records had vanished. Into the historical vacuum flowed the Bari legend and its story of medical grace emerging from wartime carnage. The story that was too good to check became a commonplace in the medical literature.
Only recently have researchers undertaken to nail down the details of the J.D. case. Michael Kashgarian, a retired professor of pathology at Yale, was one. For assistance in his hunt, Kashgarian recruited Yale School of Medicine colleagues Robert Udelsman, chair of the surgery department, and vascular surgeon John Fenn. At the same facility where J.D. underwent treatment—known since 1965 as Yale-New Haven Hospital—the men sifted pathology records from the early 1940s. The search rubric was simple: look for patients whose last names began with D and whose first names began with J. Only one hit involved a patient diagnosed with lymphosarcoma. However, that man’s medical record numbers contained errors, barring the trio from tracking down his paperwork. Sequencing the records and correcting the numbers, an archivist set the project going again. Udelsman and Fenn kept digging. In May 2010, at an off-site facility where the university stores old records, they found the papers.
“It was all there,” Fenn said. “In one patient, there was the revelation that cancer would respond to chemical injections.” The files even included sketches of J.D.’s lymph nodes. Fenn and Udelsman unveiled the details in 2011 as part of a celebration of Yale Medical School’s 200th anniversary.
“J.D. gave us hope for the future,” Fenn said. “This one patient was responsible for the birth of medical oncology.”