Dr. Shadid dared to imagine that affordable quality health care should—and could—be accessible to all.
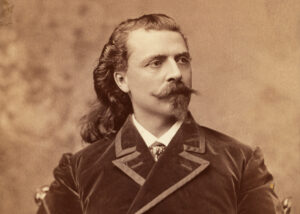
For 20 years, Michael Shadid lived the life of an Oklahoma country doctor. It was a vocation that required a young man’s endurance. Shadid trekked through dust storms and blizzards, often arriving at a dilapidated shack to perform surgery by candlelight. By his own estimation, Shadid delivered some 3,000 babies in their homes, long before hospital births became the norm. In 1928, however, well past 40 years of age, Shadid was ready for a less arduous position. He moved with his wife and six children to Elk City, a town of 6,000 people on the edge of the Dust Bowl where he enjoyed a thriving practice as a general surgeon with a small, eight-bed hospital of his own.
Medical science had advanced rapidly during those years: The doctor’s basic tools, once the stethoscope and the thermometer, now included an arsenal of expensive apparatus. It pained Shadid to watch the gap widen between those who could afford decent medical care and those who could not. Few were as vulnerable as the Oklahoma farmer, who could lose his land over the cost of an operation. It was in this milieu more than 75 years ago that the foreign-born doctor dared to imagine that affordable quality health care should—and could—be accessible to all.
Shadid intimately understood the connection between poverty and poor health care. Of the 12 children born to his family in Judedeit-Merj-ayoun, a mountain village in Lebanon (then a district of the Turkish-held province of Syria), only Michael and two siblings survived their infancy. He never knew his actual birthday, as there was “as little regard for vital statistics as for sanitation in Judedeit.” Occasionally Dr. George Post from the Syrian Protestant College of Beirut visited the area to treat the poor, and his work inspired Shadid to study medicine. In 1898, around the age of 16, Shadid immigrated to New York. He worked his way west as a peddler, selling trinkets door-to-door and saving money to pursue his dream of becoming a doctor. Upon completing medical school at Washington Uni-versity in St. Louis and serving two years as a physician’s assistant in Missouri, Shadid settled in Oklahoma in 1908.
“There must exist some unknown germ, some filterable virus unknown to man, that bites certain persons in this world and turns them into reformers,” Shadid once wrote. “I’m willing to admit that I must have been bitten early and hard.” Oklahoma in the early 20th century seemed like a good place for a reform-minded physician to be. Shadid had been active in Socialist politics, and the Socialist Party in Oklahoma was one of the strongest in the country. However, Shadid’s idea for a progressive approach to health care stemmed more from the state’s tradition of farm cooperatives than party ideology.
Several agrarian interest groups coalesced in 1906 as the Oklahoma Farmers’ Union, which gained financial equity for farmers through cooperative, group-owned entities such as cotton gins or wheat elevators. After Shadid moved to Elk City in 1928, he envisioned a cooperative hospital—what would become the first medical co-op in the United States—where members could receive comprehensive care, including check-ups and other preventive measures usually denied the poor. By charging each member an annual fee, doctors could receive regular salaries. A salaried practitioner, he reasoned, was not financially dependent on a diagnosis or a procedure. While he was a physician’s assistant, Shadid had watched an incompetent but greedy practitioner butcher an old man’s extended bladder, improvise stomach surgery on a patient suffering from an ulcer and bungle a hysterectomy—all in one night. All three patients died, and the grisly night would haunt Shadid for the rest of his life.
At the outset, Shadid hoped to include other local doctors in his cooperative, as well as the town’s two main hospitals, as such an alliance would bring in a larger membership. But the doctors wanted no part of the venture. Shadid fared better with the state Farmers’ Union, which encouraged farmers to invest in memberships at $50 per share. (At the time, a farmer typically paid $100 to enter a cotton gin cooperative. Shadid figured they would be willing to make a similar outlay for affordable health care.) The sale of 1,000 shares, Shadid calculated, would raise enough capital to build a hospital.
Although the goal was to provide comprehensive care, initially membership entitled patients to discounted medical services, including 50 percent off doctor bills, which would certainly save them more money than the $50 membership cost. To help particularly cash-strapped farmers, membership was made available at $10, with the $40 balance due in 12 months. During the summer of 1930, with 700 shares sold, construction began on the hospital.
Now that Shadid’s vision was becoming a reality, other local doctors felt compelled to take action against this potential threat to their livelihoods. In the pages of the Elk City Press, they publicly disassociated themselves from Shadid and the hospital. Privately they alleged that Shadid was a fraud intent on bilking the farmers. Such propaganda severely inhibited membership sales. By the end of December, construction had come to a halt.
In 1931 the Beckham County Medical Society met in secret to discuss expelling Shadid, a 20-year member, from the group. The society also considered bringing him before the state Board of Medical Examiners on charges of steerage—the unethical solicitation of patients—because he had commissioned agents to sell the $50 hospital memberships. A hearing could have cost Shadid his license to practice. “You and I know that people want something for nothing,” said one doctor who reported charging $50 for a tonsillectomy and $150 for an appendectomy. “And it seems to me that these dues as he calls them are but a little more than nothing.” “I am not going to tolerate foreigners coming over here and telling us how to practice medicine,” said another, ignoring Shadid’s three decades in America. One elderly physician dismissed the Community Hospital as “impractical,” predicting that it would fold in two years or less.
Impractical, perhaps, but Shadid was determined. Through a $15,000 loan secured by a term life insurance policy, along with an additional $10,000 advance of his own, Shadid resolved the financial shortfall incurred by unsold memberships. And, despite the best efforts of the Beckham County medical elite, the Community Hospital was finally ready for patients by August 1931. Three thousand Oklahomans arrived on opening day, crowding the grounds around the two-story brick building, feasting on barbecued beef served to celebrate the occasion.
Governor “Alfalfa” Bill Murray was a friend of the Farmers’ Union, which meant that he was a friend to the Community Hospital. Murray asserted in the Blue Valley Farmer that any member of a professional “inner circle” who threatened to revoke the license of a Community Hospital doctor would be prosecuted for conspiracy. Thus the rumblings within the medical society about Shadid were effectively quashed.
Still, a doctor who was ostracized by his local or state medical society faced serious consequences. He could be denied malpractice insurance, or at least charged exorbitant premiums. Other area hospitals could refuse to admit his patients. Shadid’s most immediate obstacle was staffing the hospital. Not one doctor in Oklahoma dared to rankle the medical establishment by practicing at Community Hospital. Out-of-state doctors who expressed an interest in the hospital routinely failed the licensing exam administered by the Board of Medical Examiners, which was made up of members of local medical societies.
Doctors who, on the other hand, withheld their intentions to move to Elk City stood a fair chance of passing the exam. Unfortunately, those doctors who chose to run the “medical blockade,” as Shadid called it, were as likely driven by desperation as by bravery. One doctor with excellent recommendations turned out to be a morphine addict. He managed a few days of conscientious service, only to fall into a dope-deprived panic, whereupon he swallowed poison, collapsed on the hospital floor and died soon afterwards.
In January 1932, Shadid learned that the Great American Insurance Company, which had agreed to a $15,000 loan, was sending out a representative to inspect the hospital. Since only one bed was occupied, Shadid feared that the lenders would think the hospital was financially unsound, so he enlisted his children and their friends as “patients.” The ruse worked, and the loan was secured. “It is true that I resorted to deception,” Shadid wrote later. “But I did it only because I was convinced that the hospital would ultimately succeed.”
During the early years of the Depression, Oklahoma seemed especially cursed, as nature itself menaced a land already reeling from economic disasters. Crops withered; cattle choked to death in blinding dust storms. Even with Community Hospital’s low rates, many patients couldn’t pay their bills and the hospital was operating at a loss. Shadid realized that a new payment system was needed. In 1932 he managed to convince those who were still scraping together a living that prepayment, rather than discounted service, was necessary. The hospital charged annual dues of $12 for an individual and $25 for a family of four. Hospitalization cost $1 a day; an additional $20 would be charged for a major operation. Despite the hard times, Shadid enrolled hundreds in the new plan and, over the next few years, even managed to expand the hospital to meet the growing demand for affordable care.
Still, the Oklahoma medical establishment continued to fight Shadid. They sponsored a bill to ban cooperatives in the 1936 legislative session, but it was never introduced. Then B.F. Oliver, a hospital janitor from nearby Sayre, signed a complaint charging Shadid with steerage, unprofessional conduct and fleecing the public. Shadid and his lawyer, Gomer Smith, suspected the county medical society had put Oliver up to making the complaint. If the charges proved false and Shadid decided to sue, he’d win little compensation from the janitor. The Beckham County doctors, however, had much more to lose.
Farmers rallied to support Shadid. “We think more of the few dollars invested in the Community Hospital than any investment we have ever made,” said one farmer. “I think this bunch fighting [Shadid] should be sat down so hard it would jar their ancestors for four generations.” R.M. McClintock, a political columnist for the Daily Oklahoman, shared the sentiment. “The Elk City doctor…is no quack. For years he was an honored and successful practitioner in Elk City….The fact that the hospital has had to be enlarged three times would seem to indicate that, on the whole, it is filling a real need.”
The issue finally came to trial on February 10, 1940. “In house frocks, overalls and Sunday clothes, a cross-section of Western Oklahoma took the day off to attend the most significant hearing the Beckham County district courtroom has entertained in years,” reported the Daily Oklahoman. A crowd of 500 squeezed into the courtroom, which had been built to accommodate 200. Another 1,500 of Shadid’s supporters assembled outside the building. “Of all these two thousand heads of families, these doctors could have found someone to say they’d been fleeced, besides one of their own janitors,” Gomer Smith told a reporter. The judge found the charges to be unsubstantiated, and Shadid’s license was never threatened again.
Community Hospital was the first medical co-op in the country, but it was not the only organization that proposed affordable health care through a prepaid plan. In 1929 the Ross-Loos Clinic in Los Angeles worked out a $2-a-month benefit plan for the employees of the city’s Department of Water and Power. Trinity Hospital in Little Rock, Ark., also offered care for $2 per month. Justin Ford Kimball, an administrator at Baylor University in Dallas, devised a prepaid hospitalization plan for the city’s teachers. The benefit was later extended to local newspaper and bank employees, and today it is recognized as the prototype of Blue Cross.
The organizations were responding to a problem identified by the Committee on the Cost of Medical Care (CCMC): Working and middle class consumers could not afford modern medicine. The CCMC, a privately funded group of 50 doctors, economists, scholars and other professionals, investigated the health care system nationwide between 1927 and 1932. The study found that commercial insurers typically avoided “sickness insurance,” fearing that it would only attract the ill. Anything resembling health insurance was mostly restricted to mill or mine workers who were treated by company-employed doctors.
But any attempt to manage medical services through group plans met opposition from the American Medical Association (AMA). Although 35 CCMC members endorsed a report recommending group plans, nine dissenters—eight of them doctors—issued a separate minority opinion: “Wherever [group plans] are established there is solicitation of patients, destructive competition among professional groups, inferior medical service, loss of personal relationship of patient and physician, and demoralization of the professions. It is clear that all such schemes are contrary to sound public policy.” The Journal of the American Medical Association even invoked the specters of communism and socialized medicine, calling doctors who supported group plans “Medical Soviets.”
The AMA’s attempts to undermine cooperative medicine came under government scrutiny in 1938 when a federal grand jury indicted the organization on charges of “conspiracy in restraint of trade.” Shadid was among those who testified. The AMA was convicted of violating the Sherman Anti-Trust Act for allying Washington, D.C., medical institutions against the Group Health Association (GHA), a cooperative that served low-income government employees. The move effectively prevented GHA doctors from hospitalizing their patients in the city. The AMA appealed all the way to the U.S. Supreme Court, which upheld the conviction in 1943.
In the end, World War II, not government censure, finally induced the AMA’s tolerance toward group practice and managed care. Price and wage controls, enacted to contain inflation, impelled employers to offer health benefits to attract workers during a period of extremely low unemployment. According to Paul Starr, author of The Social Transformation of American Medicine, the number of people covered by hospital plans between 1942 and 1945 grew from less than 7 million to 26 million, with Blue Cross dominating the market.
A clarion call for greater access to health care for all Americans was heard in President Harry S. Truman’s address to Congress on November 19, 1945. Truman quoted Selective Service data stating that nearly 5 million male draft registrants between the ages of 18 and 37—some 30 percent of all those called up—had been classified as unfit for duty because of “physical and mental incapacity.” It was a sobering assessment of the nation’s health.
Truman pushed for a five-point plan that included building hospitals in underserved areas; expanded public health, prenatal and child care programs; medical education and research; prepayment of health care costs; and protection against lost income because of illness or injury. The president was quick to assure the American people that he wasn’t advocating socialized medicine. Doctors would not become government employees, Truman said, and patients would still be free to choose their doctors and services. The only difference would be that getting care “would not depend on how much [patients] can afford to pay.”
Truman won allies among legislators, unions and religious and civic organizations. But his initiative made little headway after Democrats lost control of Congress in the 1946 midterm elections. Still, it had substantial public support. When the National Health Assembly met in Washington in May 1948, some 850 representatives from organized medicine, public health, labor and other interests outlined a 10-year plan to improve health care. Surprisingly, the AMA formally acknowledged the benefits of cooperatives and other prepayment plans during this progressive assembly, although it held fast against compulsory national health coverage.
When Truman won the presidential election six months later, the AMA promptly launched a full-scale public relations campaign to win the hearts and minds of all those Americans who stood with the president and his vision of health care. In pamphlets, radio spots, print ads and other media, the AMA hammered home its message: “In America, We Don’t Like Compulsion!” “When You’re Sick, Do You Want Doctors—Or Clerks?” “Political Medicine Is Bad Medicine.”
The AMA endorsed inexpensive, voluntary plans such as Blue Cross and its younger cousin, Blue Shield, which offered limited coverage for doctor bills as an alternative to government-administered compulsory insurance. The most destructive salvo was the AMA’s allegation that Truman’s plan was indeed “socialized” medicine, and therefore a portal for communism to infect the government. The news was rife with stories about Reds infiltrating society; the smear fit with the tenor of the times. While Truman’s proposals languished in Congress, unions were winning comprehensive health care for thousands of workers through collective bargaining, thus weakening labor’s stake in—and support for—national insurance.
Despite the AMA’s grudging acceptance of cooperatives, back in Elk City the Beckham County Medical Society continued to resist Community Hospital. By 1950 the hospital served 2,400 families, but it re-mained difficult to attract qualified professionals to an institution held in disrepute by the medical establishment. In August, the hospital filed suit against the county society, citing “conspiracy in restraint of trade,” the same charge that the Justice De-partment had used to indict the AMA in Washington 12 years earlier. An out-of-court settlement in 1952 finally permitted Community Hospital doctors to join the society, entitled to all the privileges attending their hard-won respectability.
Shadid retired from Community Hospital in 1946 and remained an advocate for cooperative medicine, writing, lecturing and serving as the first president of the Cooperative Health Federation of America. But his progressive ideas did not resonate during the prosperous 1950s as they had during the Depression. Community Hospital ceased operating as a cooperative in 1955, a year when 70 percent of Americans held health coverage. Today it is the Great Plains Regional Medical Center.
It was a conceit of those optimistic years that corporate medicine and commercial insurers would fill the need once met by maverick physicians. Today, the AMA estimates that one American in seven does not have health insurance, and the vast majority of the uninsured come from working families. Affordable quality health care will again be an issue in the 2008 presidential campaign as doctors, insurers, politicians and the public seek relief from skyrocketing costs and limited access.
Dr. Shadid would find the scenario all too familiar. Recalling a family that he had treated for typhoid at reduced rates, Shadid was deeply touched by their gratitude. “But they should never, in my opinion, have been put in the position of having to feel grateful for something they should receive as a right,” he said. “It is our Christian and patriotic duty to give every American the best medical care his country has to offer.”
Steve Boisson has written for Writer’s Digest and the Boston Globe. This story appeared in the April 2008 issue of American History.