![[National Archives; Photo illustration by Guy Aceto]](https://www.historynet.com/wp-content/uploads/image/2013/WWII/10%20Oct/penicillin.jpg) During the First World War, tens of thousands of service personnel die—not from physical damage caused by their wounds, but of sepsis, a massive body-wide infection. The medical profession is almost powerless to prevent these deaths, but during and after the war an impassioned search gets underway to discover an effective treatment. One physician absorbed in this effort is bacteriologist Alexander Fleming, at Saint Mary’s Hospital in London. Fleming traces the inspiration for his quest, in part, to his wartime experiences as a captain in the Royal Army Medical Corps seeing hundreds of wounded men perish from sepsis.
During the First World War, tens of thousands of service personnel die—not from physical damage caused by their wounds, but of sepsis, a massive body-wide infection. The medical profession is almost powerless to prevent these deaths, but during and after the war an impassioned search gets underway to discover an effective treatment. One physician absorbed in this effort is bacteriologist Alexander Fleming, at Saint Mary’s Hospital in London. Fleming traces the inspiration for his quest, in part, to his wartime experiences as a captain in the Royal Army Medical Corps seeing hundreds of wounded men perish from sepsis.
In September 1928 Fleming makes a startling discovery. Upon returning from vacation, he discovers that he left uncovered a petri dish in which a staphylococcus culture was growing. Accidental exposure to the air has contaminated the dish, and a blue-green mold has begun growing in its medium. Oddly, this mold has a ring around its perimeter devoid of staph bacteria. Fleming discerns that something in the mold must be inhibiting—in fact preventing—the bacteria from growing. He identifies the mold as penicillium, a fungus, and after some experimentation isolates the element in penicillium that is responsible for this effect. He calls that element penicillin.
Fleming experiments with penicillin and publishes a paper on its effects, but lack of time and resources inhibits him from undertaking major trials. These are finally done in the late 1930s, when fellow bacteriologists Howard Florey and Ernst Chain conduct the first sustained experiments with penicillin. Although the drug’s scarcity prevents the other Britons from achieving any real breakthrough, Florey and Chain are able to demonstrate that the antibiotic is effective in mice and causes no harm to humans.
Human studies produce cures in persons with infections. The results are sufficiently promising that, soon after World War II begins, British researchers urge their American counterparts to be more aggressive in pursuing penicillin research. The antibiotic sees its first major use in the U.S. on hundreds of people burned in a catastrophic fire at the Cocoanut Grove nightclub in Boston in November 1942.
Success at reversing infection in the Boston burn patients persuades the War Production Board to underwrite major research by pharmaceutical firms, universities, and especially the Department of Agriculture’s Northern Regional Research Laboratory. That facility, in Peoria, Illinois, has been studying penicillin since June 1941.
However, a substantial roadblock bars mass production of the penicillium mold from which penicillin is derived. Researchers devise a means of surface fermentation that grows mold, but the process is hopelessly slow and inadequate.
As a result, a pound of penicillin costs $45,000 ($711,830 today). To cure a single infection can require two million units of penicillin. In addition, the drug does not linger in the body, which flushes it in only a few hours. Doctors prize penicillin so dearly that they collect the urine of patients treated with it to recover the excreted antibiotic so they can purify and reuse what otherwise would go to waste.
Efforts to synthesize penicillin fall short. Chemical engineers are able to identify the molecular structure but not to mimic it in substantial amounts. Ultimately the War Production Board withdraws support for penicillin research in favor of obtaining improvements in sulfanilamide, a synthesized compound that was the first commercial antibiotic drug and is capable of halting infections but not reversing them. Pharmaceutical manufacturers produce “sulfa” in enormous quantities and the drug, in powder and tablet form, is administered to wounded men in all theaters of the war, often sprinkled onto wounds during combat.
The above scenario is accurate in most respects. Fleming did indeed discover penicillium’s antibiotic properties. Florey and Chain did indeed conduct important research. The War Production Board did spend heavily to underwrite mass production and synthesis of the drug, and surface fermentation did prove inadequate to the task of mass production. Penicillin’s initial costliness is also a historical fact, as is the practice of extracting and repurposing penicillin recovered from patients’ urine. The extensive use of sulfa is also accurate.
The chief departure from history concerns a crucial breakthrough: creation at the Peoria labs of a process in which scientists grew penicillium mold in large drums that were constantly agitated and aerated. The “deep fermentation” method tremendously increased the surface area the mold needed to flourish, with a concomitant dramatic rise in the amount of extractable penicillin. The lab was also able to isolate high-yield penicillium strains, helped considerably by discovery of a mold growing on the skin of a locally harvested cantaloupe that contained the richest presence yet of penicillium.
As a result, penicillin production ballooned. The amount of the antibiotic made in July 1943, for example, equaled the total output achieved during the previous six months. As plants came online to manufacture penicillin in volume, supply rose from 21 billion units in 1943 to 1,633 billion in 1944, and a whopping 7,052 billion units in 1945. Penicillin thus became a practical cost-effective drug.
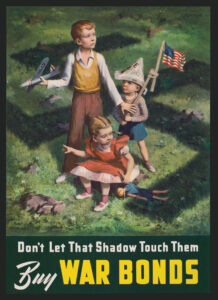
The military began using penicillin in the spring of 1943, when pilot studies persuaded the U.S. Army to purchase 150 million units per week for hospital use. By 1944 the army was receiving 85 percent of all American penicillin output. The first personnel to benefit were in the Eighth Air Force; within a few months, penicillin was seeing use in every theater of the war. The drug played a particularly important role during and after the Normandy landings in June 1944 as Allied troops fought their way east across Europe.
Central to this amazing success story was the deep fermentation process developed at Peoria by chemical engineer Margaret Hutchinson Rousseau. But what if Rousseau had failed to discover and perfect deep fermentation? The theoretical cost of that failure can be measured by penicillin’s historical success. Among American military personnel, the drug cured roughly 95 percent of wound infections. The antibiotic was also effective against most of the sexually transmitted diseases that historically had sapped the armed forces. Now men infected by carnal misadventure often could return to duty.
“With the war’s definitive wonder drug available to treat wounds and disease,” medical historian Albert E. Cowdrey explains, “American fighting men had a greatly increased chance of surviving injury.” By one estimate, 10 to 15 percent of wounded U.S. servicemen eluded death thanks to the availability of penicillin.
The drug also obviated the need for many amputations, because in combination with surgical procedures penicillin could neutralize the bacteria that caused the gas gangrene responsible for earlier eras’ myriad limb removals.
Penicillin became one of the great medical success stories of the twentieth century. But this never would have happened without the ability to mass-produce it. Thousands of personnel who escaped death or amputation owed their well-being to the deep fermentation process that paved the way for mass production, to the chemical engineer who developed the process, and even to a moldy cantaloupe harvested somewhere in Peoria, Illinois.