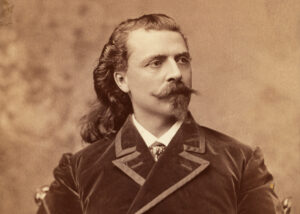
James O. Finnegan
Lt. Cmdr., M.D., U.S. Navy Reserve
3rd Marine Division
Sept. 1967-Sept. 1968
My father was 27 with two kids when Japan bombed Pearl Harbor. As much as he tried to join the military, his job as a foreman in a Pittsburgh steel mill was deemed vital to the war effort. Haunted by the fact that he never finished high school and did not serve, my dad would tell me, “I don’t care what career you choose, but you must go to college and you must serve your country.” When I was accepted into med school in 1960, his only question was about when I would find time to serve in the military. By mid-1967 I knew that I had the medical and surgical skills that could help those wounded in combat. I told the Navy that I’d relinquish my deferment to finish residency training if they would guarantee me a billet as a surgeon with the Marines. By September 25, I was in Vietnam.
I was the triage surgeon on duty at Dong Ha combat base in late November 1967 when we got word that casualties were on their way. A CH-46 and a CH-53 Jolly Green Giant landed in front of the triage building. Four KIAs were taken to Graves Registration and 14 litters of the most seriously wounded were put on iron horses. I quickly appraised each, putting the worst wounded in the first position, the rest placed according to injury severity.
A Marine named Lopez had wounds so severe that he got the first slot. He was in profound shock from heavy blood loss, had no obtainable blood pressure, and was extremely pale and cold, but I was certain I felt a pulse. The anesthesiologist put a tube into his lungs and began manual respirations as the team checked every inch of his body.
Remarkably, though he had multiple wounds over his body, there were no head or face wounds. Another corpsman confirmed that Lopez had no obtainable blood pressure. I opened his left chest, put the rib retractor in place, opened the pericardium, or heart sac, and began massaging his heart. The anesthesiologist breathed for him while other team members assessed and dressed his wounds. Large-bore intravenous lines were already in place, and blood was being pumped in, but we were unable to restore any hint of a pulse or blood pressure. I pronounced Lopez dead and told the litter bearers to take him to Graves Registration.
Before long, the stretcher bearers came back into triage with Lopez, swearing that he was moving. Once again we made a full resuscitative effort. Still no pulse or blood pressure. I had no choice but to pronounce the poor guy dead again.
Minutes later, four angry and very spooked Marines charged back into triage with Lopez. “This sonovabitch is moving!” they screamed. “We’re not taking him back!” By now, the whole scene was attracting a lot of attention. I called another surgeon over to assess the situation. “Jim, he’s dead, there’s nothing we can do for him,” he said. But, I couldn’t send him back to Graves Registration a third time—the Marines would go crazy. So I told him to take Lopez to the OR for surgery. “What the hell do you want me to operate on?” he asked. I told him to open Lopez’s belly to see what was going on, to just do it.
After I had triaged all of the other casualties, I went into the OR. The anesthesiologist told me that shortly after surgery on Lopez started, an EKG tracing began to appear very slowly and a bit irregularly, then a little faster and quite regularly. Despite this, he was unable to detect a blood pressure. I watched as multiple shrapnel holes in his small and large intestines were repaired. After about 30 minutes, the anesthesiologist suddenly yelled that he thought he was, in fact, hearing a slight blood pressure. He continued pumping blood and fluids into Lopez. Moments later, he said he was clearly hearing something at about 80/50. By the time the abdominal portion of the procedure was over, Lopez’s blood pressure was over 100 systolic, and he actually needed anesthetic to keep him asleep and comfortable! I quickly scrubbed into the surgery to close the chest incision I’d made for the cardiac massage. Lopez was moved to the intensive care unit in critical condition, but was maintaining a good pulse and blood pressure on his own.
 When we arrived in the ICU the following morning, Lopez’s breathing tube had been removed and he was breathing comfortably on his own. The next day, he was medevaced to Da Nang. I never saw him again.
When we arrived in the ICU the following morning, Lopez’s breathing tube had been removed and he was breathing comfortably on his own. The next day, he was medevaced to Da Nang. I never saw him again.
Everyone at Dong Ha knew what had happened. But the good feeling that permeated the base could never compare with the sense of accomplishment felt by the corpsmen, physicians and surgeons of the 3rd Medical Battalion. For me, it was a profound lesson in humility and a powerful reminder that we don’t have all the answers. I knew that the experienced combat surgical team assessed him not once or twice but three times, and by all measurable criteria Lopez was dead. I ordered him to surgery instinctively, on a purely emotional basis. The will to live and the power of the spirit will always be one step ahead of us—with Lopez.
Dr. Finnegan later commanded a surgical team that treated 2,500 Marines during the siege of Khe Sanh. He is now a Philadelphia area surgeon and recently published his memoir: In the Company of Marines, A Surgeon Remembers Vietnam.